What Should I Expect as Dementia Progresses?

How dementia progresses
Receiving a dementia or Alzheimer’s diagnosis can be shocking. You or your loved one will probably feel overwhelmed. What does this mean for you and your family? What does this mean for your daily life?
While everyone’s journey with Alzheimer’s is different, doctors have identified the progression of the disease in five stages. Knowing these stages and what to expect in each one can help you prepare for living with Alzheimer’s or caring for a loved one who is.
Share this Infographic Image On Your Site
<p><strong>Please include attribution to https://thebreckinridge.com/ with this graphic.</strong><br><br><a href="https://thebreckinridge.com/ways-to-stay-engaged-socially-with-dementia/"><img src="https://thebreckinridge.com/wp-content/uploads/2022/11/2-taking-on-the-role-as-a-care-partner-for-someone-with-dementia-thebreckinridge.jpg" alt="Taking on the Role as a Care Partner for Someone with Dementia" width="1200px"></a></p>What to expect during the five stages of dementia caused by Alzheimer’s disease
1. Preclinical Alzheimer’s disease
This stage begins before symptoms of Alzheimer’s appear, such as memory loss or changes in personality and behavior. With advanced research, we now know that Alzheimer’s can appear in the brain long before the disease is noticeable to you or others. Because of this, you may not notice any change in yourself or a loved one during this stage as symptoms aren’t evident.
If Alzheimer’s or dementia runs in your family, you may opt to have genetic testing to see if you carry a common genetic mutation that is linked to Alzheimer’s disease. You can also talk to your doctor about blood testing and brain imaging that can detect Alzheimer’s at its earliest stages.
2. Mild cognitive impairment due to Alzheimer’s disease
The Mayo Clinic defines mild cognitive impairment (MCI) as “the stage between the expected cognitive decline of normal aging and the more serious decline of dementia.”
MCI can be caused by Alzheimer’s disease or other conditions such as nutritional deficiencies, autoimmune disease, metabolic imbalance, a brain tumor and more. MCI typically causes issues with thinking, reading, learning, remembering, reasoning and attention span but not to the degree that these issues interfere with daily tasks and activities.
If you’re noticing any signs of MCI, don’t write them off as normal symptoms of aging. Seek a proper diagnosis from a geriatrician or neurologist to determine if MCI is being caused by Alzheimer’s or another condition.
3. Mild dementia due to Alzheimer’s disease
This is the stage when Alzheimer’s is most commonly diagnosed because this is typically the stage when symptoms become evident to you, your loved one or a doctor.
Symptoms of mild dementia due to Alzheimer’s disease include:
- Short-term memory loss: difficulty remembering recent events or information
- Poor judgment: making poor decisions due to a loss of sound judgment and reasoning skills
- Difficulty with problem-solving or completing tasks: an inability to do complex tasks such as balancing a checkbook and an inability to follow through with daily tasks after they are started
- Misplacing items: misplacing valuable items more frequently and not being able to remember where they are
- Change in personality: withdrawing in social gatherings or feeling angry or irritable more often
- Getting lost more frequently: getting lost on the way to places that were once familiar
These symptoms indicate that memory loss and other symptoms have begun to interfere with daily life, making the disease much more prominent and noticeable.
If you haven’t already, you will want to seek out a proper diagnosis at this time and establish a plan of care. Talk to your doctor about your options for medication, therapies and other treatments.
This is also a good time to start planning for your future if you are the one living with dementia. This way you can feel empowered in your choices and how you want to live as the disease progresses. Establish whether or not you will want to move into a long-term care facility during the later stages of the disease or if you prefer full-time, at-home care. Determine who will be power of attorney and handle future affairs, and make sure your will is in order.
This is also a good time to seek support. Counselors and therapists are available for those who are living with Alzheimer’s as well as caretakers. There are also support groups available for caretakers and those who have loved ones living with Alzheimer’s or dementia. These can be incredibly helpful resources as you face the unknown of your disease or take on new responsibilities as a caretaker. To find support near you, contact your local Alzheimer’s chapter here.
4. Moderate dementia due to Alzheimer’s disease
At this stage of Alzheimer’s, the symptoms that began in the mild dementia stage grow more severe. Memory loss and confusion increase. Basic personal details, like your birthday, may become difficult to remember. Personality and behavior changes are more evident at this stage. Many grow suspicious of their caretakers and loved ones or think they are seeing or hearing things that aren’t there.
At this stage, most will need help with activities of daily life (ADLs), such as going to the bathroom, changing clothes and eating. Because of this, you or your loved one may need to transition into a memory care facility that offers full-time care, or you may need to hire assistance in the home.
Be sure to talk to your doctor about all treatment options available at this stage. The Alzheimer’s Association also provides information about resources in your community that can help assist you or your loved one during this time. Contact your local chapter to learn more.
5. Severe dementia due to Alzheimer’s disease
Throughout every stage of Alzheimer’s disease neurons in the brain are deteriorating, shrinking the brain. During the final stage of Alzheimer’s, the disease has affected every area of the brain needed for daily functioning. This makes communication difficult and assistance with all ADLs is usually required. It can also become difficult to move or sit up on your own. Eventually, someone with severe dementia due to Alzheimer’s will lose the ability to swallow and control his or her bowels.
Because Alzheimer’s is a degenerative disease of the brain, it is ultimately fatal. You will want to have an end-of-life plan in place for your loved one and be sure to have plenty of support during this time.
As we mentioned above, if you have dementia, don’t delay in telling your loved ones what your wishes are as your disease progresses. Will you be ok with moving into a facility or would you prefer at-home care? Who do you want to handle your affairs? Is your will in order? These are difficult questions to ask and equally difficult to answer, but when you and your family are on the same page about your plan of care, you can rest easy knowing your wishes will be fulfilled and everyone will know what to do when the time comes.
How fast does dementia progress?
Now that you understand the stages of Alzheimer’s, you’re probably wondering how long it takes for the disease to progress. While doctors can make estimates based on various factors, the progression of the disease solely depends on the individual. The average life expectancy for someone with Alzheimer’s is eight to 12 years from the time of diagnosis, though people have lived up to 26 years after their diagnosis, especially if they are diagnosed early.
Because of this, knowing exactly how quickly the disease will progress can be difficult to estimate. However, there are factors that can cause the disease to move more quickly.
What causes dementia to progress quickly
1. Age

More research is needed to conclude if age causes dementia to progress more quickly, but there is evidence to support that if you are diagnosed with Alzheimer’s before age 65, known as early-onset Alzheimer’s, the disease is likely to progress more quickly than if you are diagnosed over the age of 65.
This could be due to the fact that early-onset Alzheimer’s is largely associated with genetics while late-onset Alzheimer’s can be caused by a number of factors, so these two types of Alzheimer’s may have pathological differences that cause one to progress more quickly than the other.
2. Preexisting health conditions

If you already have heart disease, diabetes or high blood pressure at the time of diagnosis, Alzheimer’s may progress more quickly, especially if these conditions have not been managed well. A healthy heart is essential for a healthy brain, and an unhealthy heart can do a lot of damage to the brain, especially if you have Alzheimer’s.
3. Delirium

Delirium is a condition that begins suddenly in someone who may already have dementia. Delirium causes you to feel confused and can be very distressing. Bouts of delirium can cause Alzheimer’s disease to progress more quickly.
4. Stroke
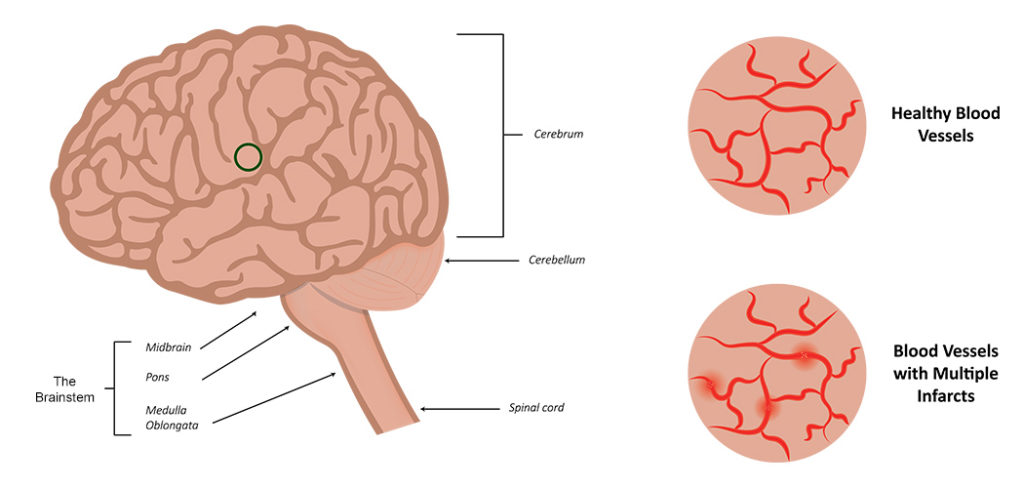
Those with vascular dementia (a type of dementia associated with decreased blood flow to the brain that almost always coincides with Alzheimer’s disease) are at higher risk for stroke. Having a stroke when you already have Alzheimer’s disease can cause the disease to progress more rapidly because strokes cause further damage to the brain.
No matter where you are in your Alzheimer’s journey, be sure to have a plan of care in place for now and the future. Make sure family members are on board with the plan and understand the wishes of the person living with Alzheimer’s. While the disease can make you feel out of control of your life and future, there are many things you can do to ensure you or your loved one feels empowered in their choices, prepared for what’s the come and equipped to live the best life possible with dementia.