How Does Dementia Change Behavior?

If you’re a caregiver for someone with dementia or the loved one of someone with dementia, you have probably noticed a change in this person’s behavior. That’s what tipped you off to his or her dementia in the first place.
The most noticeable and tell-tale sign of dementia is memory loss. This is the symptom most often associated with dementia and Alzheimer’s. But dementia includes an array of symptoms that affect someone’s behavior, not just memory loss.
Behavioral changes caused by dementia include:
Regardless, it’s important to know that behavioral changes in someone with dementia are normal, should be expected and shouldn’t be judged or reacted to harshly. People with dementia need empathy and understanding. They are navigating the world in a completely new way. This is very disorienting. The better you can understand their experience, the better you will be able to handle and care for these behavioral changes.
Why does dementia affect behavior?
Dementia affects behavior for a number of reasons, the top being:
Losing neurons in the brain
Dementia and Alzheimer’s cause neurodegeneration in the brain, which is a deterioration of cells. Because our brains are what affect our behavior, anything that causes cells to break down in the brain will cause our behavior to change.
For dementia, changes in behavior depend on which area of the brain is being affected.
Areas of the brain associated with dementia and Alzheimer’s
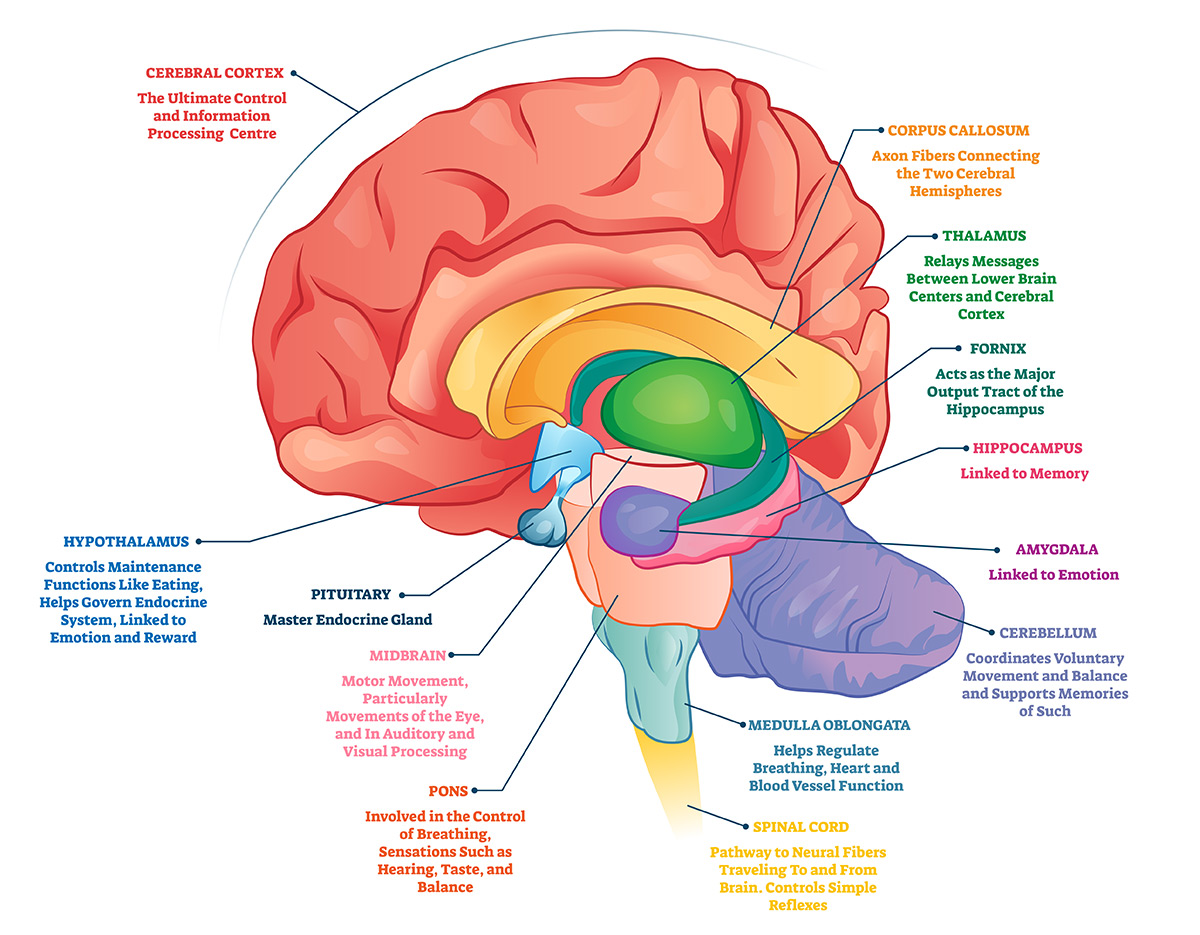
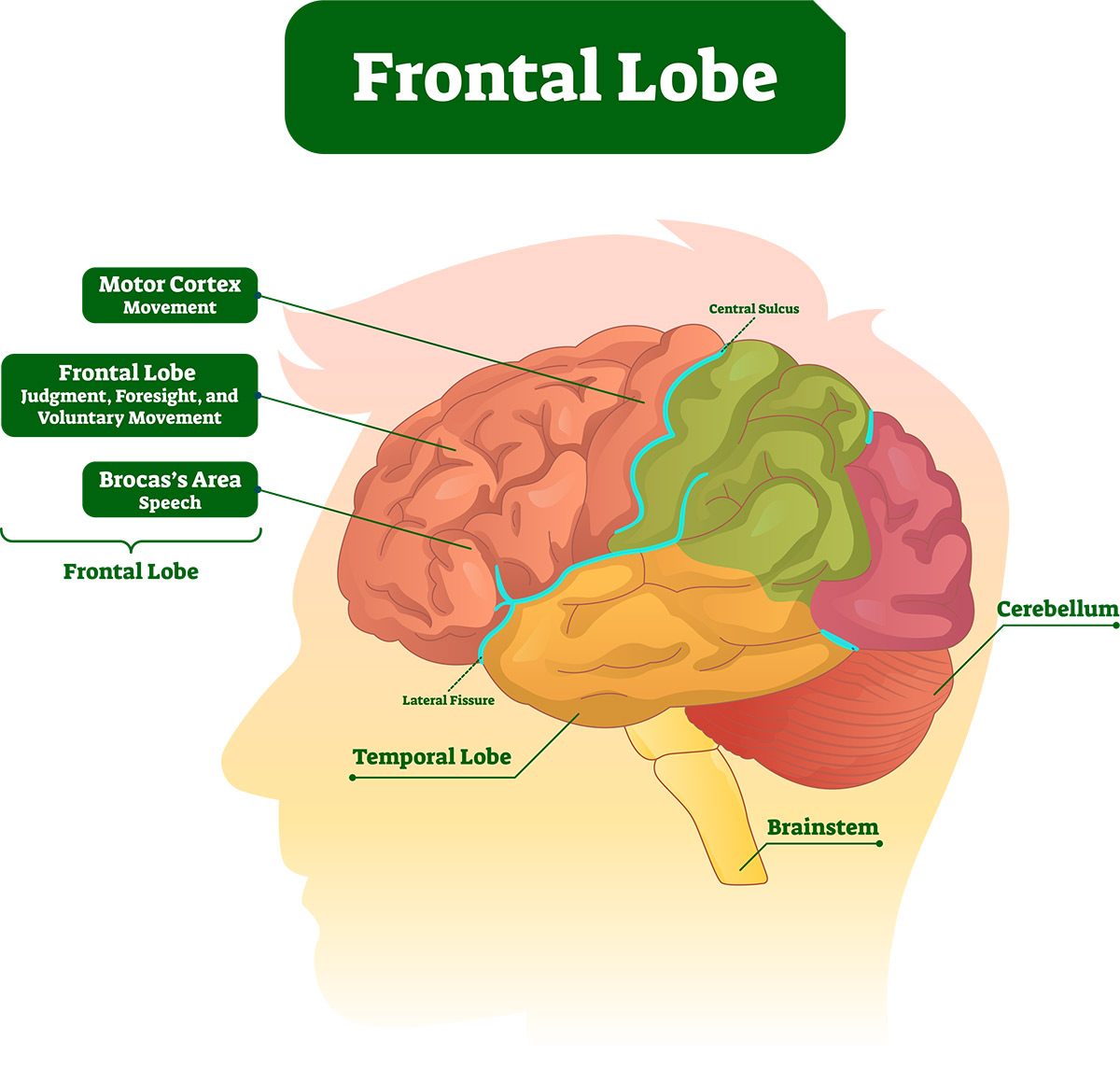
The frontal lobe is responsible for thinking, memory, behavior and movement.
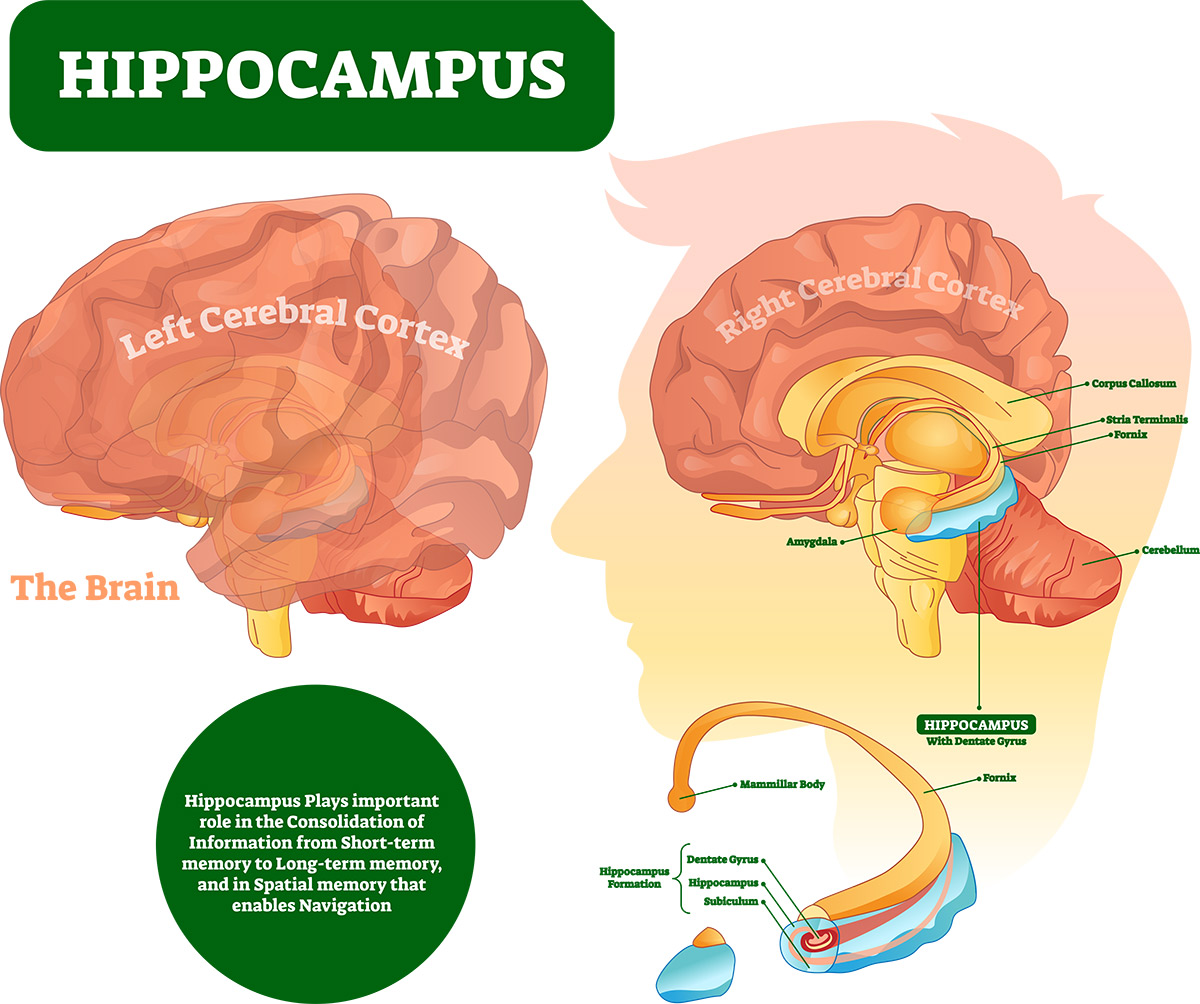
The hippocampus is responsible for memory retrieval. (Because short-term memory is affected more than long-term memory for those living with Alzheimer’s, the hippocampus is associated more with retrieving short-term memories.)
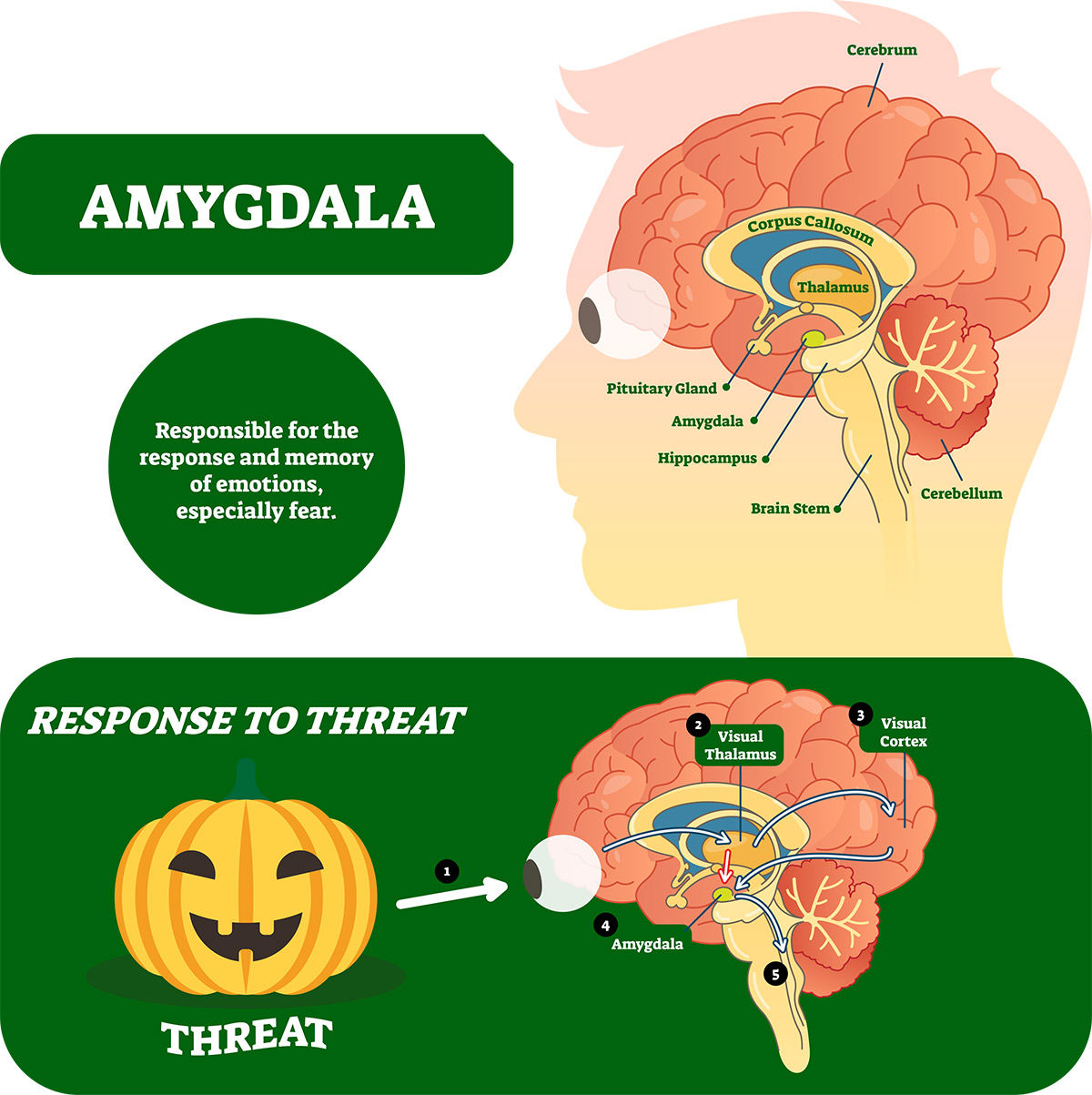
The amygdala is responsible for our emotional responses. (This area of the brain is typically affected later than the hippocampus for those with Alzheimer’s disease.)
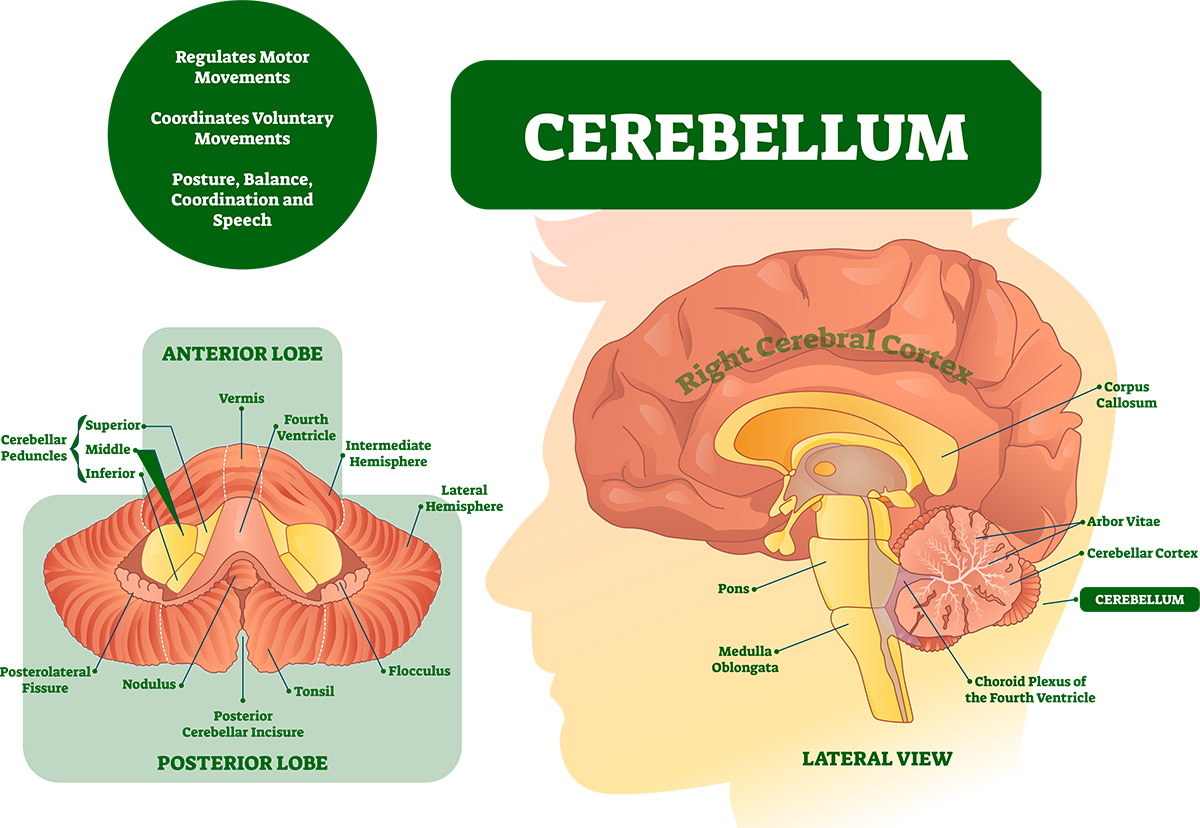
The cerebellum is responsible for balance and coordination. (Vascular dementia is known for causing issues with balance.)
Depending on where the degeneration in the brain is occurring, that is where you will likely see behavioral changes.
Environmental effects
People with dementia can be greatly affected by their physical and emotional environment. If they are in a noisy or crowded place, they can easily feel overwhelmed. If they are trying to follow a conversation but having difficulty due to confusion or their attention span, they may become agitated.
People living with dementia also pick up on the emotions of those around them. So if you’re feeling anxious or worried, they might notice that and also feel anxious or worried.
Of course if the above is true then so is the opposite. People with dementia thrive better in a calm environment surrounded by people who are patient and not easily irritated. Regular routines and schedules are also helpful for behavioral symptoms of dementia.
Medical Issues
With dementia come other medical issues, both physical and emotional. Those with dementia often develop anxiety or depression due to their diagnosis or neurodegeneration. They may also develop an infection such as a urinary tract infection that they aren’t able to communicate clearly. They are in pain but can’t tell you why. This may cause them to feel anxious, agitated or to lash out.
Medication can also cause side effects for those with dementia, causing changes in their behavior.
Communicating physical, psychological and social needs
One of the most difficult parts of dementia, for those living with dementia and for caregivers, is the inability to effectively communicate needs. People who are living with dementia don’t have the communication skills they once had. Their memory and language are greatly affected by the disease. When they are uncomfortable, hungry, thirsty, sick or tired, they may not know how to tell you this. Instead, they may get angry or agitated. They may shut down and not communicate at all.
This can be very frustrating for caregivers but is the area where caregivers must pay closest attention because being in tune with your loved one’s needs will allow you to meet those needs and, therefore, help the challenging behavior in the moment as well as help prevent it in the future.
Physical needs
Like all of us, people with dementia have physical needs. If they’re not able to get these needs met, their behavior may change. They might become agitated, angry or confused.
Physical needs that can be difficult to communicate for those with dementia include:
If your loved one is showing signs of aggression, agitation or is shutting down, consider if any of these physical needs are not being met and how you could meet them. Once their basic physical needs are met, their behavior will change.
Psychological needs
While you may feel confused about your loved one’s behavioral changes, they are most assuredly more confused. They are experiencing life in a new way. They’re not able to do the things they once could. All of this can lead to great emotional and psychological distress, causing depression, anxiety, delusions and hallucinations.
If you’re noticing any of these psychological changes, talk to a professional. Therapy and counseling can be helpful for the psychological distress caused by dementia.
Social needs
People living with dementia often feel lonely or isolated. Due to their diagnosis, they might pull back from social activities or conversations, afraid they won’t be able to participate like they once could. Even though they may fear social interactions or be tempted to avoid them, being around other people and feeling socially connected is crucial for those with dementia.
In addition, due to isolation, they may feel bored because of a lack of stimulation. If they watch T.V. all day or sit in the same place, they will need more stimulation for their senses.
Be aware of your loved one’s social needs. They may need to be encouraged to socialize or they may need help getting out of the house for stimulating activities.
How you can deal with behaviors that are challenging
When you’re caring for someone with dementia who is exhibiting challenging behaviors, the DICE tool can be helpful.
D
Describe what happened.
What did they do?
What was the effect of the behavior?
Is safety a concern?
I
Investigate possible causes.
What need isn’t being met?
C
Create a plan.
How could you meet that need or ask someone else to help you meet that need?
E
Evaluate the plan.
Was your plan effective?
Did you get to the root of what they needed?
What do you need to do differently next time to help prevent this behavior?
Behavior that requires more intervention
Most dementia-related behavior is innocent and can be dealt with if you understand the underlying cause of the behavior.
However, certain types of behavior might require more intervention such as:
If your loved one is showing any of the above behaviors, the Memory and Aging Center of the University of California San Francisco offers a helpful list of how to respond to each behavior here. You can also call the Alzheimer’s 24/7 helpline at 1.800.272.3900.
If you’re a caregiver or the loved one of someone living with dementia or Alzheimer’s, their behavioral changes can be difficult at first.
You feel like you’re losing the person you love. But know that these changes are inevitable with this type of disease. It’s not that you’re losing the person you love so much as you’re losing the way this person used to communicate. They, and you, simply must find improvements in their behavior.