What Are The 7 Stages of Frontotemporal Dementia?

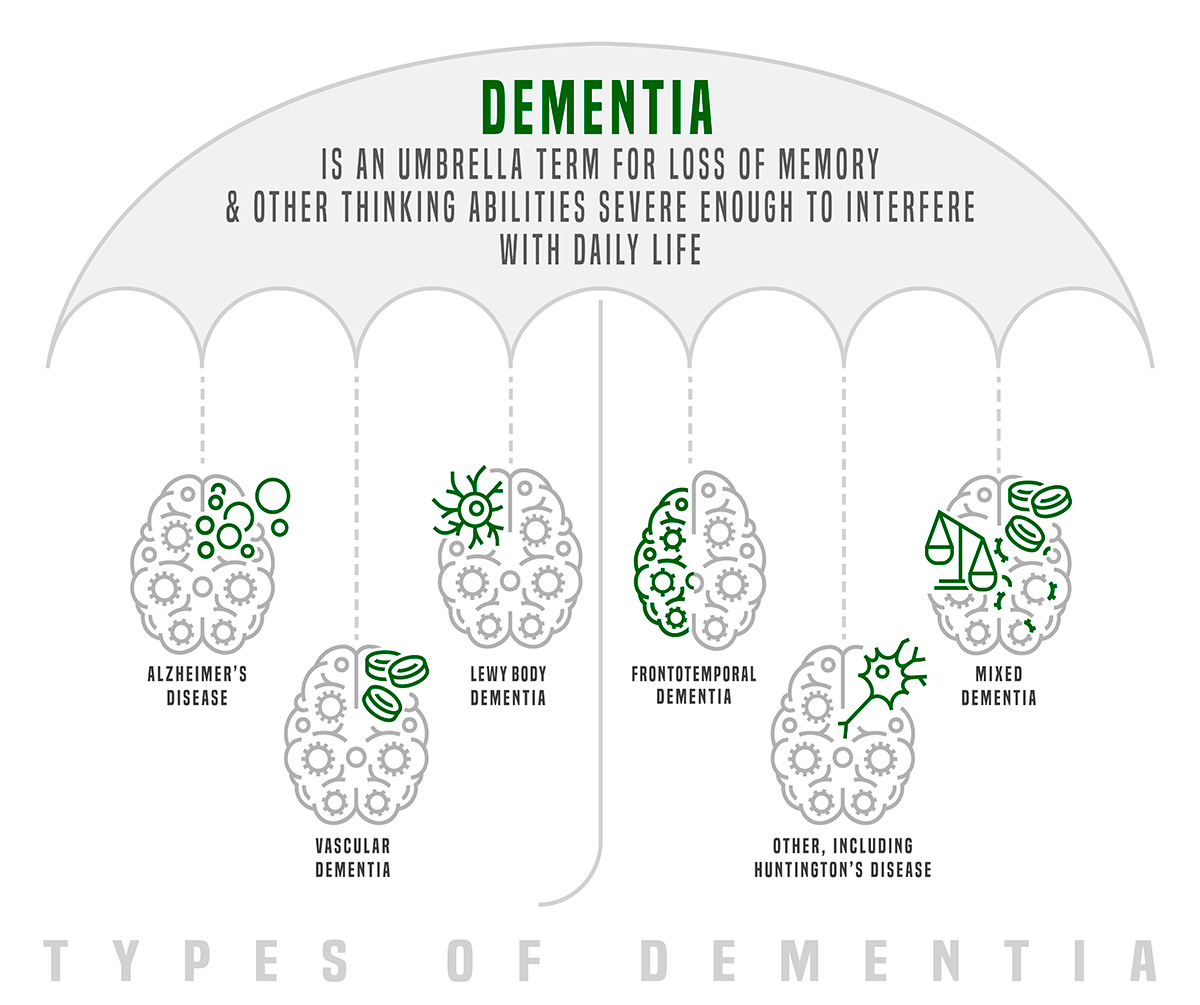
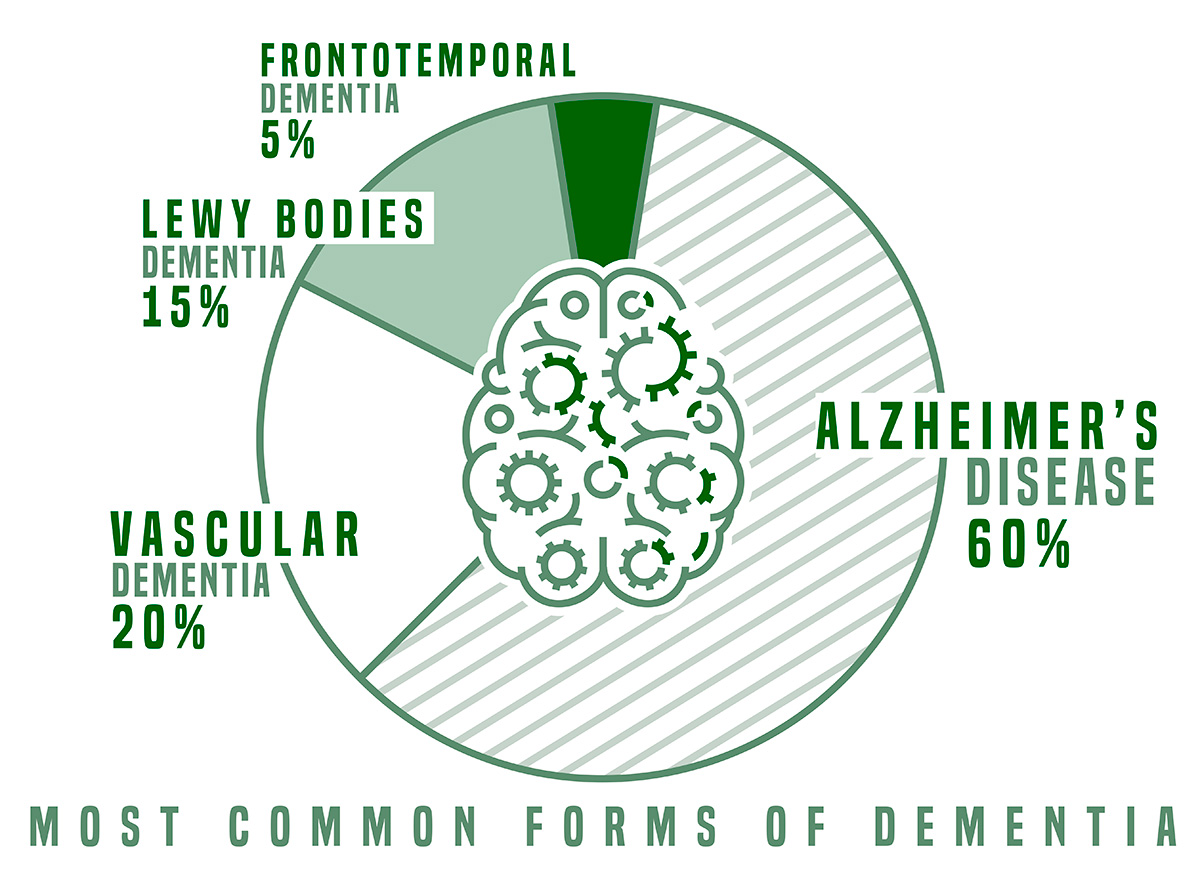
While dementia education and awareness have greatly increased in the last decade, Alzheimer’s is still the most broadly discussed and understood form of dementia. But dementia can take many different forms, affecting different parts of the brain and following different patterns of progression. One lesser-known form of dementia has been in the news more frequently due to a celebrity diagnosis.
Last year, actor Bruce Willis announced he had been diagnosed with frontotemporal dementia (FTD), a type of dementia that affects the frontal and temporal lobes of the brain. Since then, awareness of this type of dementia has increased and hopefully will continue to do so as symptoms of FTD can be difficult to identify in its early stages.
What is frontotemporal dementia?
Frontotemporal dementia is caused by protein build-up in the frontal and temporal lobes of the brain, which are responsible for language and behavior. Because of this, early symptoms of FTD are typically associated with behavior and personality changes or language problems.
FTD typically shows up earlier than Alzheimer’s, with the average age of diagnosis between 45-65. There are a few different types of FTD that will determine whether speech and language or personality and behavior are affected most, but general symptoms include:
What are the 7 stages of frontotemporal dementia?
According to Dementech Neuroscience, a private mental health clinic that specializes in neurodegenerative diseases, someone with frontotempora dementia will progress through seven stages of the disease, moving from mild to moderate to severe. How long each stage lasts will vary by person and depends on a number of factors, including preexisting health conditions, medications, age of diagnosis and lifestyle.
Stage 1: Mild Cognitive Changes
Frontotemporal dementia is difficult to detect at this stage. While changes are happening in the brain, these changes may only show up as slight behavioral or personality changes—not enough to alarm family and friends and often mistaken for natural changes that occur with aging.
Stage 2: Changes in Behavior
Subtle changes in behavior continue in this stage as well as problems with language and speech. Someone may become less inhibited in public, acting inappropriately, or they may have trouble finding the right word to use. While frontotemporal dementia remains difficult to detect at this stage, close family or friends may begin to suspect a problem.
Stage 3: Difficulty with Language
At this stage, frontotemporal dementia becomes more apparent. While the person with frontotemporal dementia may not notice a change, those around him probably will. Language becomes more difficult at this stage and these challenges start to affect his everyday life at work, at home and in public interactions.
Stage 4: Greater Impact on Quality of Life
Language continues to decline at this stage but becomes more obvious as simple words can be difficult to remember once frontotemporal dementia has progressed to this point. Being unable to communicate effectively can dramatically impact every area of life, so this is when many who are living with frontotemporal dementia begin to experience a reduced quality of life. Some may also struggle with memory at this stage, and behavioral changes and issues will continue to increase in frequency and severity.
Most likely the person living with frontotemporal dementia will not notice these changes in themselves, making it difficult for caring friends and family to get them the help they need.
Stage 5: Personality Changes
At this stage, the symptoms of frontotemporal dementia become more severe, sometimes mimicking Alzheimer’s disease. Someone living with frontotemporal dementia at this stage may start to have difficulty with memory and problem-solving. They will often start to need help with activities of daily living like eating and bathing, and they may start to exhibit issues with motor skills, such as swallowing.
Stage 6: Loss of Memory
At this advanced stage of frontotemporal dementia, symptoms worsen, often making a memory care facility or nursing home necessary. Memory, language and motor skills continue to decline and falls become more common. Those living with the disease become less responsive and appear to be “locked inside themselves,” as Dementech explains.
Stage 7: Severe Cognitive Decline
This is the final stage of frontotemporal dementia when existing symptoms become more severe and new symptoms can arise. There is no cure for frontotemporal dementia, but medications and therapies can help ease symptoms at this stage. While frontotemporal dementia is not fatal on its own, an illness like pneumonia can be fatal in conjunction with frontotemporal dementia, so illnesses become much more serious. Anyone living with frontotemporal dementia at this stage will require full-time care, whether at home or in a memory care facility where trained staff can keep them comfortable as they enter the final months or years of the disease.
If you or someone you love has been diagnosed with frontotemporal dementia, learning about these stages can be difficult, but being educated is crucial. It can allow you to make end-of-life plans and decisions about care while you are still able to, ensuring your wishes will be honored or ensuring you know exactly what your loved one wants as they progress through the disease.
If you have questions about memory care options, our experts at The Breckinridge are available to speak with you. Contact us here or learn more about the uncommon care we provide.