Frontotemporal Dementia Eyes: How Does Dementia Affect the Eyes?

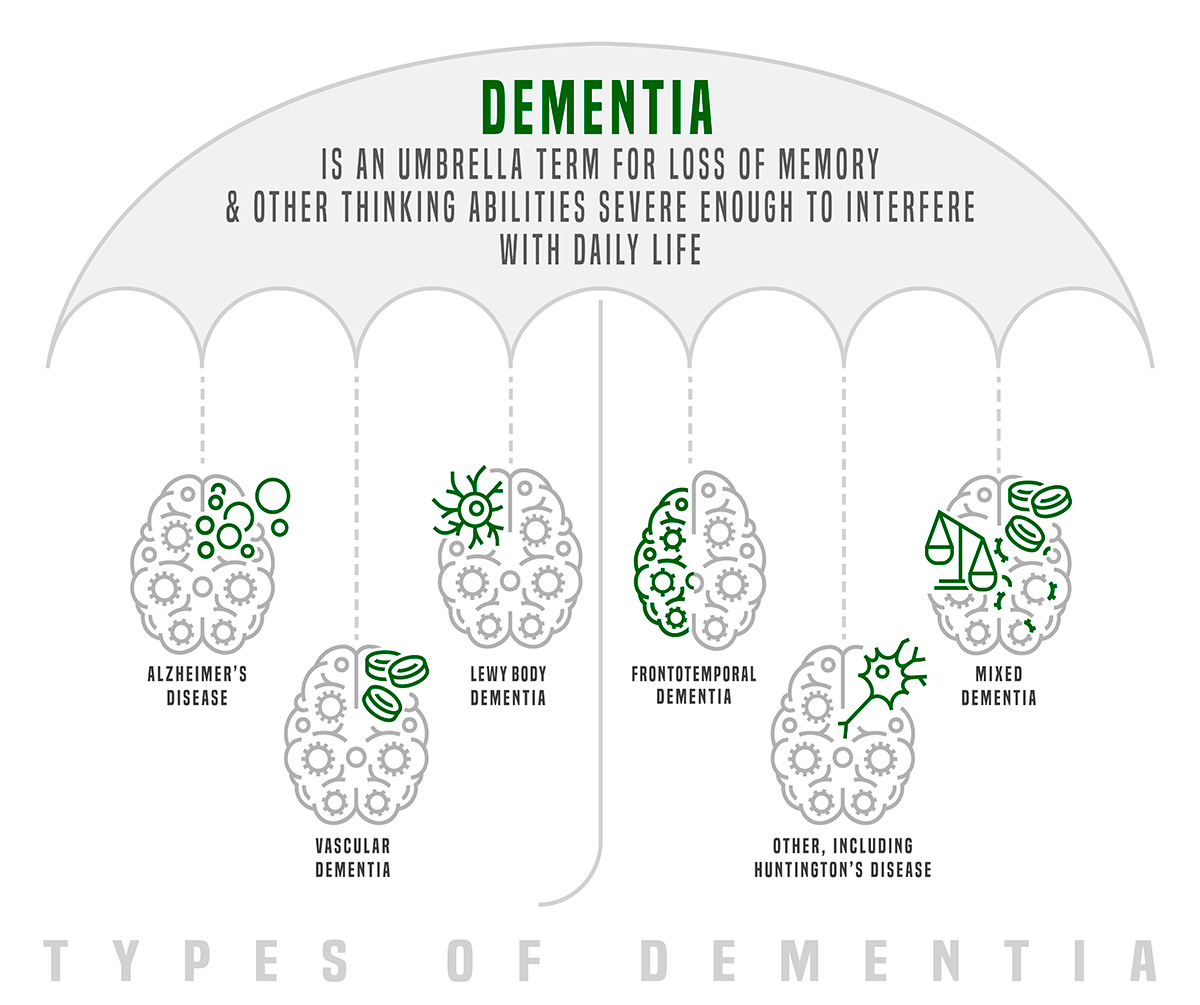
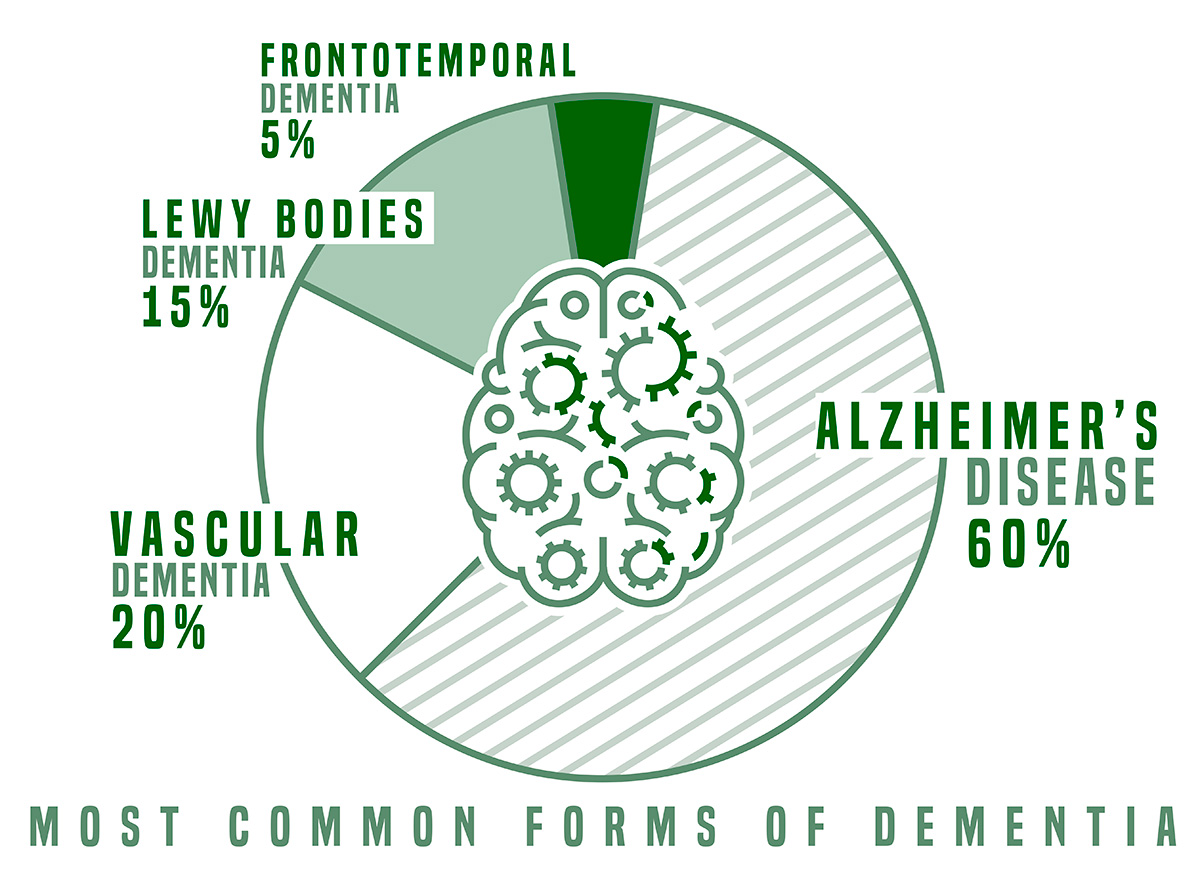
When we talk about dementia, we often talk about it as a disease of the mind. While this is true, dementia can affect every area of the body. It is not just a memory disease. The neurodegeneration caused by dementia can lead to issues with motor skills, speech and language and the deterioration of other organs, including the eyes.
Dementia’s effect on the eyes is not broadly understood and is often overlooked by caregivers who can confuse eyesight problems with other symptoms of dementia. In addition, recent studies have shown that deterioration in the eyes could be an early indicator of dementia and Alzheimer’s for those who haven’t been diagnosed and are in the early stages of the disease. Understanding the link between the eyes and dementia can help caregivers, researchers and doctors know how to better treat and diagnose Alzheimer’s and other forms of dementia.
How does dementia affect eyesight?
Eye function can be greatly impacted by the neurodegeneration caused by dementia. According to dementia care expert Teepa Snow, the field of vision for someone with progressed dementia can be as little as twelve inches. Some may experience monocular vision—when you can only see out of one eye—and others can have trouble with depth perception. Understanding the vision limitations of someone who is living with dementia can greatly affect their care.
For example, a lack of depth perception can often be confused with hallucinating, which is a symptom of some types of dementia. Someone who is living with dementia may reach for a light switch they think is close by when it is actually across the room. A caregiver may confuse this with a hallucination, thinking their loved one is reaching for something that isn’t there. In reality, the person with dementia is simply struggling with depth perception. Being aware of this distinction could prevent unnecessary prescriptions for antipsychotic drugs, which are given for hallucinations.
Vision problems for those who are living with dementia are also often confused with behavioral problems. One expert shared the story of a woman in a memory care facility who kept stealing food from others’ plates at mealtime. After investigating the situation, a dementia care consultant discovered the woman simply couldn’t see the food on her plate in front of her because her downward vision was impaired, so she was taking food she could see in her peripheral vision from other residents’ plates. Knowing the difference between a behavioral issue and a vision issue is crucial for caregivers to know how to intervene in situations like this.
Can the eyes predict whether or not someone will develop dementia?
Dementia affects eyesight, and the eyes can provide invaluable insight into dementia.
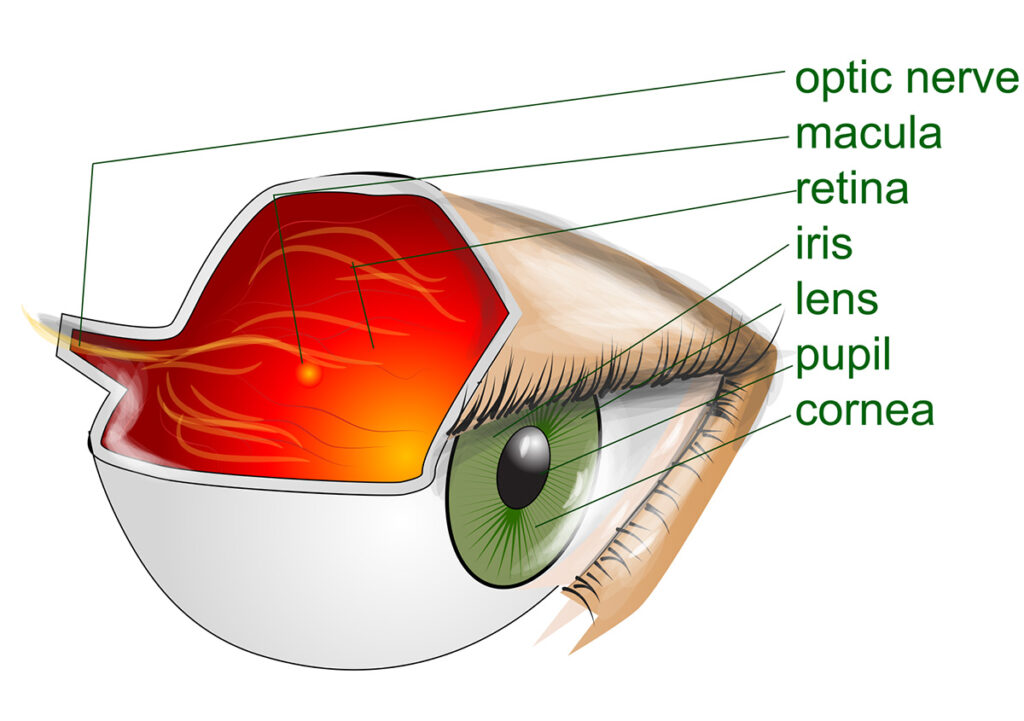
For the past several years, neuroscientists have been investigating the connection between damage to the retina—the layer of tissue at the back of the eyeball—and the likelihood of developing dementia and Alzheimer’s disease.
A study conducted by Duke Eye Center in 2019 found changes in blood vessels of the retina in those who are living with Alzheimer’s disease. Because of this, the researchers believe eye exams could help diagnose Alzheimer’s disease in the early stages. As this article explains, “Researchers believe that because the retina is an extension of the brain and shares many similarities with it, deterioration in the retina may mimic changes in the brain’s blood vessels, providing a window into the disease process.”
In a more recent study, neuroscientist Dr. Robert Rissman found that spots on the retina correlated with the presence of beta-amyloid plaque—a hallmark of Alzheimer’s disease—found on brain scans. This means these retinal spots, which can be seen during a routine eye exam, could indicate the presence of amyloid plaques in the brain. For someone who does not yet have a dementia diagnosis, this could lead to an earlier diagnosis, earlier intervention and, therefore, a higher quality of life while living with the disease.
Frontotemporal dementia eyes
Looking at the eyes can also help diagnose certain types of dementia that are often mistaken for other neurodegenerative diseases. For example, frontotemporal dementia (FTD), a type of dementia that affects the frontal and temporal lobes in the brain, is easy to misdiagnose because of its similarities to diseases like ALS. A 2017 study found that for someone with frontotemporal dementia eyes, thinning of the retina occurs similarly to those with Alzheimer’s disease or ALS but in a different location in the retina. Therefore, an eye exam can help not only diagnose dementia but the type of dementia someone may be developing.
When it comes to dementia, the eyes are indeed a window into the person who is living with it. Knowing how dementia affects the eyes can help direct the type of care someone receives. And knowing the eyes can provide clues to what is happening in the brain is helping doctors and scientists diagnose dementia and Alzheimer’s earlier and more accurately, providing hope for those who are living with the disease and those yet to be diagnosed.
Does frontotemporal dementia have a direct effect on the eyes?
Frontotemporal dementia does not have a direct effect on the eyes. However, some patients with frontotemporal dementia exhibit distinctive alterations in visual processing or eye behavior as the disease impacts certain brain regions.
These can include:
So, in essence, while the eyes themselves are unaffected in frontotemporal dementia, visual processing abnormalities emerge progressively as higher cortical and subcortical pathways controlling functions like coordinated eye movements, object recognition, and gaze control succumb to neurodegeneration. Patients struggle increasingly with processing intuitively what they see accurately.