Does Our Skin Hold Clues to Dementia?

When caring for it comes to neurological disorders like dementia, Alzheimer’s and Parkinson’s disease, the most natural place to look for early signs and symptoms is the brain. After all, these are neurological illnesses. But more and more researchers are pointing to other organs and parts of the body that may indicate early signs of neurodegeneration. These signs can be key to early diagnosis and proper treatment.
“Brain & Life” magazine recently published a story about a man whose rosacea – a common inflammatory skin disease that causes redness in the skin — turned out to be an early indicator of Parkinson’s disease.
Signs of Rosacea
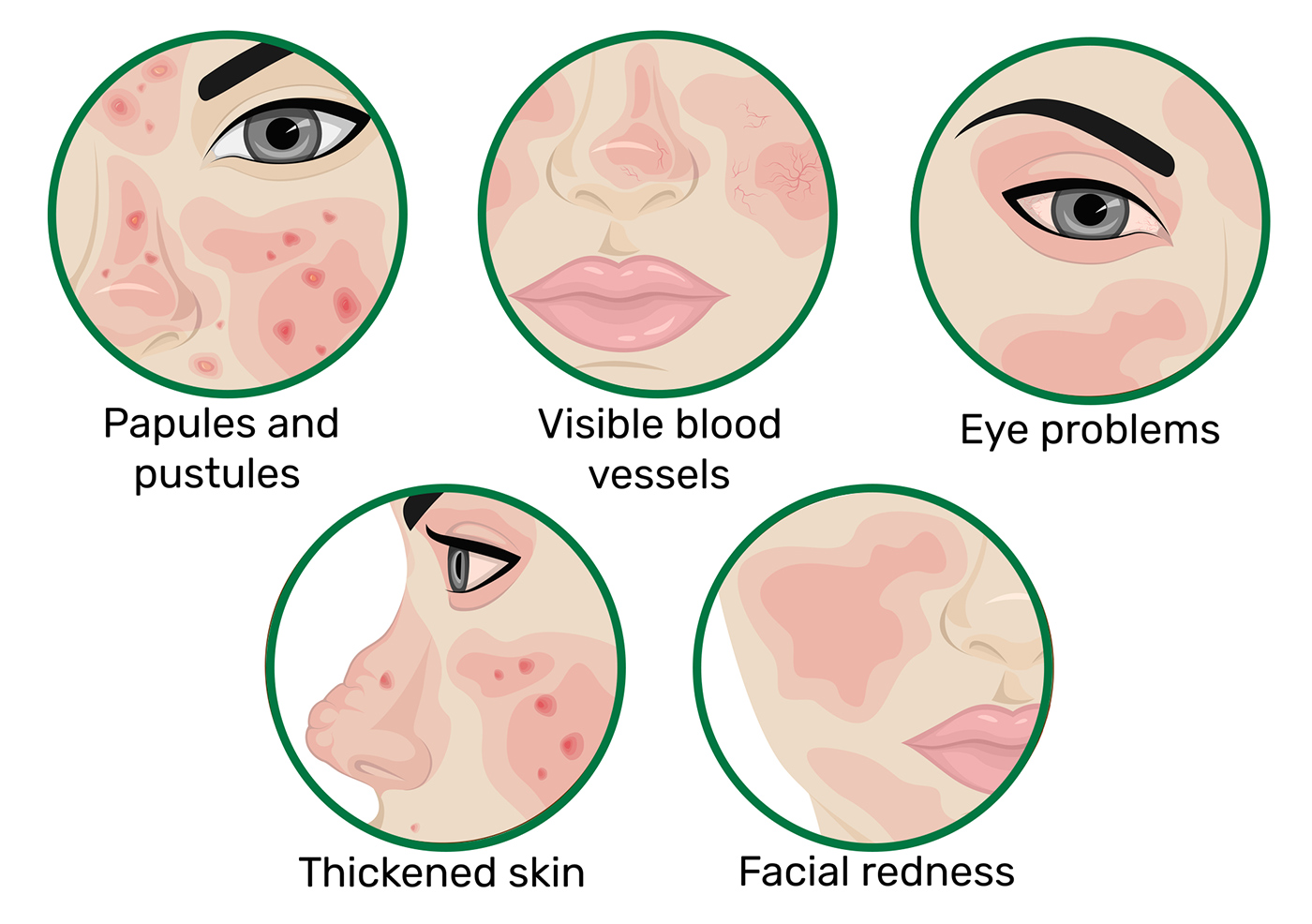
The article quotes neurologist José Biller, MD, who explained the importance of examining the skin when testing for a neurological disease. “There are literally hundreds of neurologic disorders with manifestations in the skin,” he says. This means dermatologists must work closely with neurologists, referring patients to neurologists whenever new skin conditions appear that could be linked to a neurological disorder.
Why Skin Conditions Can Be Linked to Neurological Conditions
The link between brain health and heart health is broadly known and understood. Proper blood flow to the brain is essential for the brain to function properly. If the heart isn’t pumping enough blood, the brain will suffer. But with an organ like your skin (which is often not even thought of as an organ), the link is less obvious.
According to researchers, the connection between our skin and our brains could go as far back as the womb. As Dr. Ildefonso Rodriguez-Leyva explained to the BBC, “Skin has the same origin as brain tissue in the developing embryo and might, therefore, be a good window to what’s going on in the mind in later life—at least at a molecular level.”
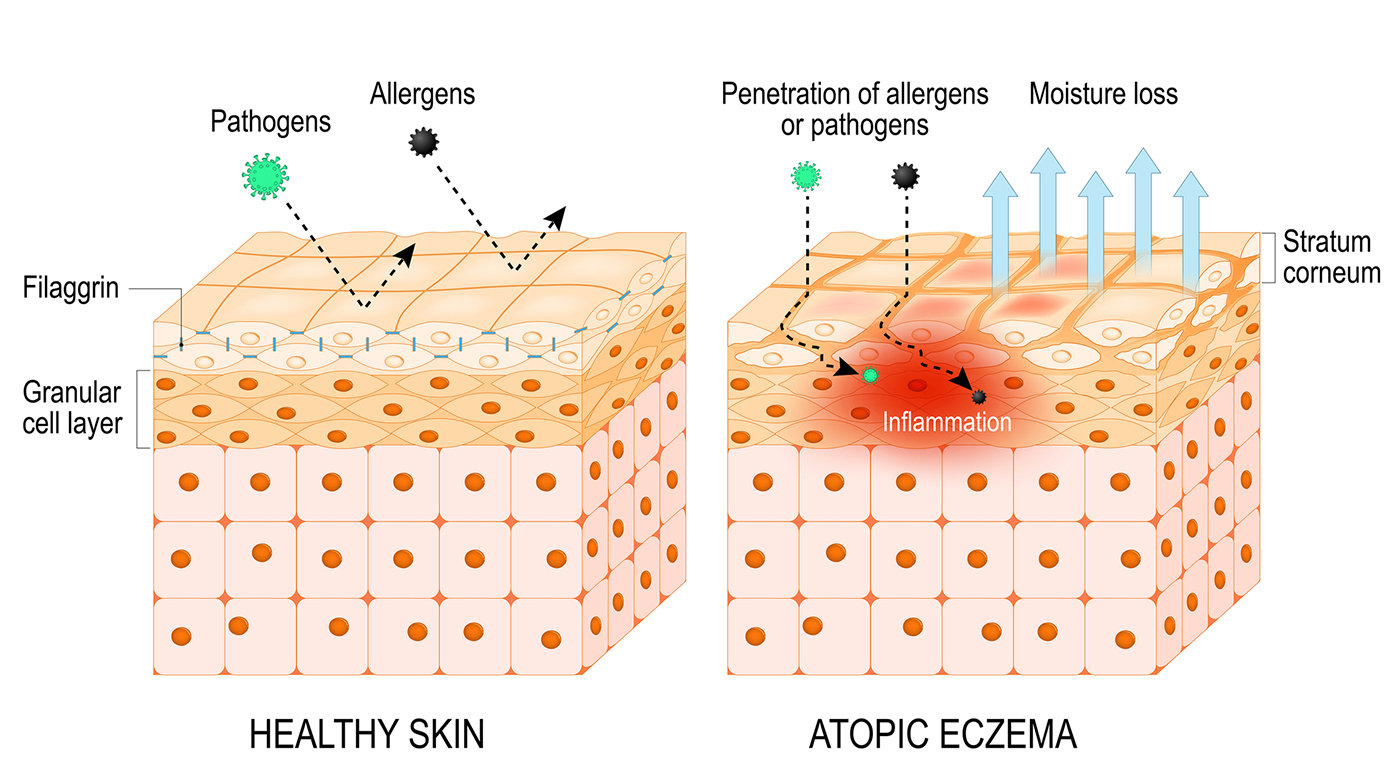
Inflammation may also be key to understanding this link. Researchers who looked at the link between atopic eczema, a skin condition that causes itchy, dry skin, and dementia believe that chronic inflammation is the reason these skin diseases often coincide with neurological illnesses. Skin conditions like eczema and chronic neurological diseases are both caused by chronic inflammation.
Skin Conditions that May Increase Your Risk for a Neurological Disease
In addition to atopic eczema, which in the study mentioned above found that the presence of atopic eczema increased the chances for older adults to develop dementia by 27%, other skin diseases have been linked with certain forms of dementia and Parkinson’s disease.
Atopic Eczema
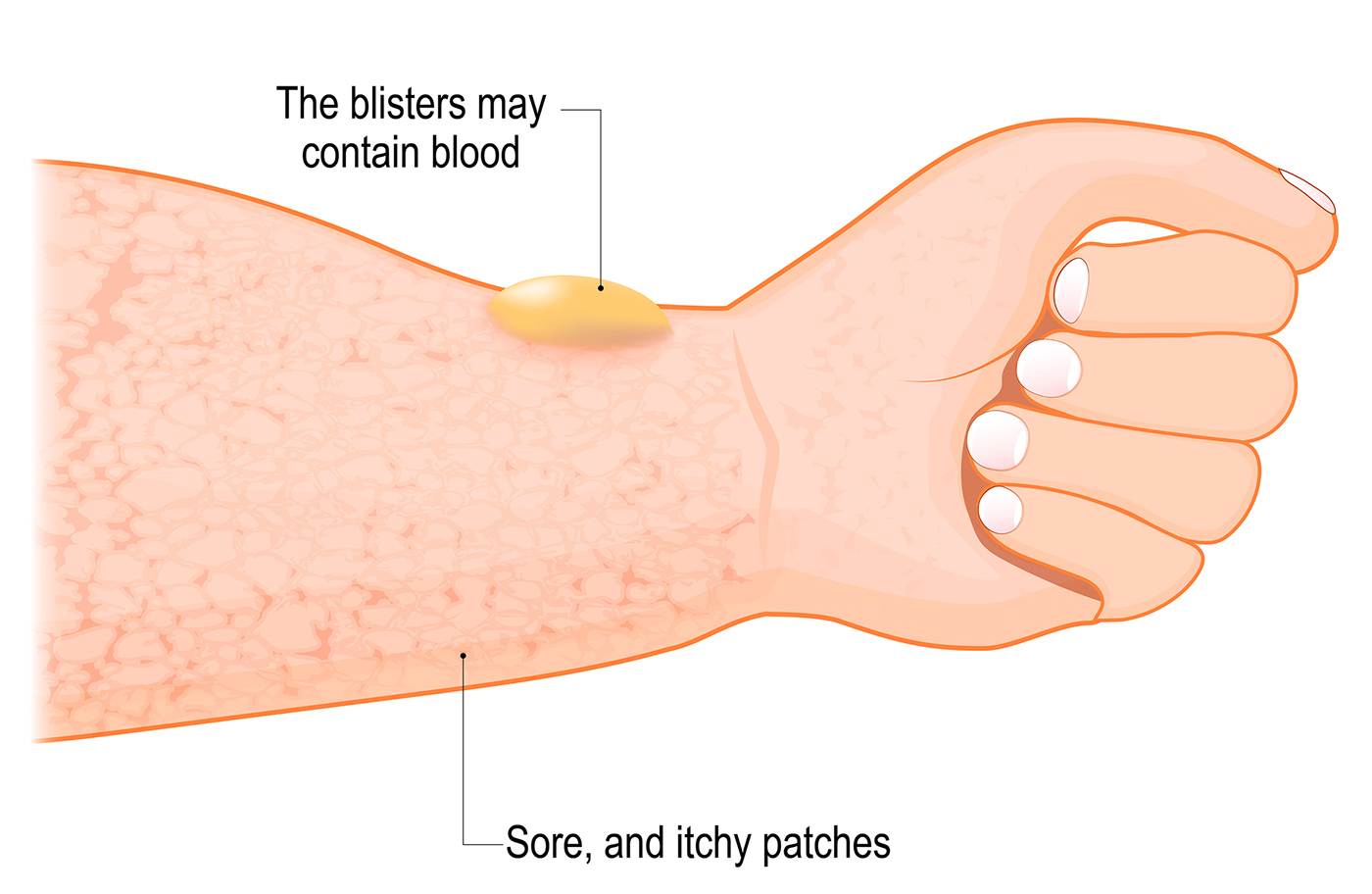
Bullous Pemphigoid
According to to “Brain & Life,” bullous pemphigoid, an autoimmune disease that causes blisters on the skin in older adults, has been linked to dementia, Parkinson’s, epilepsy, multiple sclerosis and stroke. Bullous pemphigoid can be an early indicator of a neurological disorder, or it can appear after a neurological diagnosis as a symptom rather than a sign
Bullous Pemphigoid
Psoriasis
Researchers have looked closely at the link psoriasis, an inflammatory skin disease that causes itchy, scaly patches on the skin, and Alzheimer’s disease. While studies and research have come up with conflicting results (some believe there is a link while others don’t), both diseases have inflammatory roots and share a genetic component. One study done in Korea found that psoriasis patients who received an anti-inflammatory medication were less likely to develop Alzheimer’s disease, suggesting untreated psoriasis could increase the risk for Alzheimer’s disease
Psoriasis
Occasionally, someone with dementia at the end of his life may experience moments of lucidity — a phenomenon that’s been observed months and years before death but is most often recorded in the days leading up to death. These are moments in which your loved one may suddenly remember details once forgotten — who you are, where he is, significant recent events.
These moments, while often a precursor to death, may help researchers better treat dementia and Alzheimer’s. As Andrew Peterson, a researcher of bioethics and consciousness, explains, these bursts of lucidity suggest “there may be neural networks that are remaining, and/or pathways and neural function, that could help potentially restore cognitive abilities to individuals we otherwise think are permanently impaired.”
Skin Tests as a Biomarker for Dementia
Biological markers, or “biomarkers,” are measurable indications doctors use to detect disease.
For Alzheimer’s, testing cerebrospinal fluid, the liquid around your brain and spinal cord, has become a common biomarker for Alzheimer’s. By measuring certain types of proteins found in this spinal fluid, doctors can determine if someone is at risk for Alzheimer’s disease.
Now, some experts think skin could be the next biomarker for early detection of Alzheimer’s disease.
In Mexico, researchers performed skin tests on 53 subjects who had either Alzheimer’s or Parkinson’s disease. The tests found raised levels of tau and alpha-synuclein proteins—hallmarks for Alzheimer’s and Parkinson’s disease—on the skin as well as in the brain. These findings suggest testing the skin for levels of certain proteins could help indicate the presence of a neurological disease, even before more obvious symptoms appear.
How Our Skin Could Help Properly Diagnosis Types of Dementia
While every type of dementia has its distinct characteristics, symptoms and progressions, some types can be difficult to distinguish from one another, particularly frontotemporal dementia.
Frontotemporal dementia (FTD) affects the frontal and temporal lobes of the brain, which are responsible for language and behavior. Symptoms of FTD are often confused with Alzheimer’s disease, making FTD difficult to diagnose.
A 2018 study found that skin conduction levels — a measure of electrical current in the skin—were different in those who were living with FTD versus those living with Alzheimer’s. This difference could help doctors properly diagnose FTD and better understand this disease that is so often misunderstood.
Most skin conditions are not indicative of Alzheimer’s or another neurodegenerative disease, but understanding the link between certain skin conditions and neurological disorders provides hope for dementia and Alzheimer’s research. The more we understand how this disease can manifest in different parts of the body, the better we can understand cognitive decline as a whole, what causes it, and, hopefully, one day, how to cure it.